Articles
Stories on meth addiction, sex, and recovery within the LGBTQ+ community & beyond
Embark on a Journey of Chemsex Recovery!

Fawcett Receives “Stigma Warrior” Award at International Conference
In November I was privileged to be invited to participate in a plenary session at the 15th annual International...
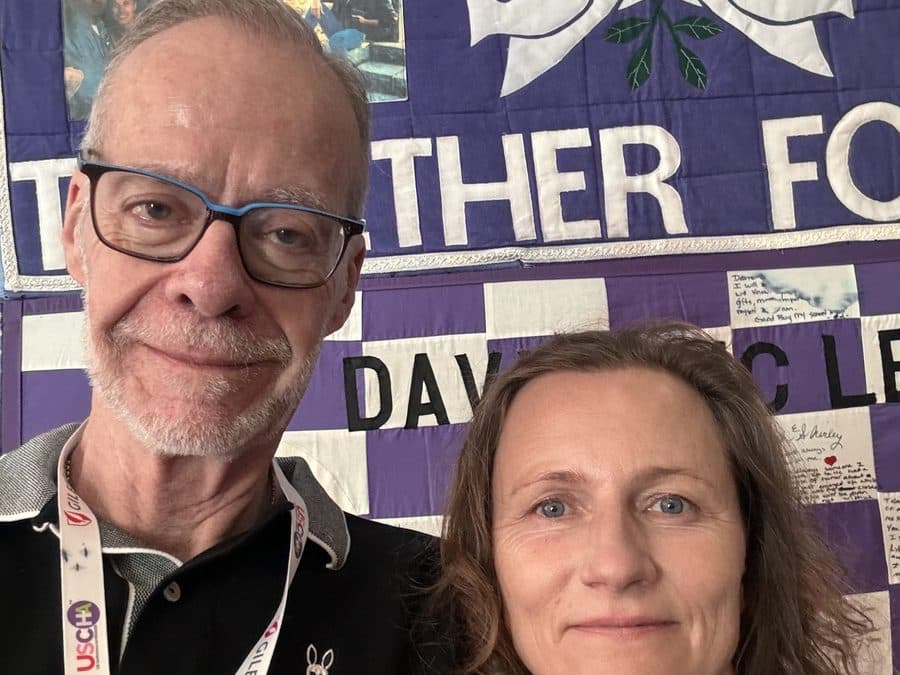
Fawcett Presents Two Workshops at the US Conference on HIV/AIDS
Despite the best efforts of Hurricane Francine, the US Conference on HIV/AIDS successfully met over the course of...

Life’s Spectrum: Support for Aging, Sex, and Intimacy among Gay Men
The Impact of the Pandemic During the pandemic many members of Fawcett’s community experienced profound depression,...
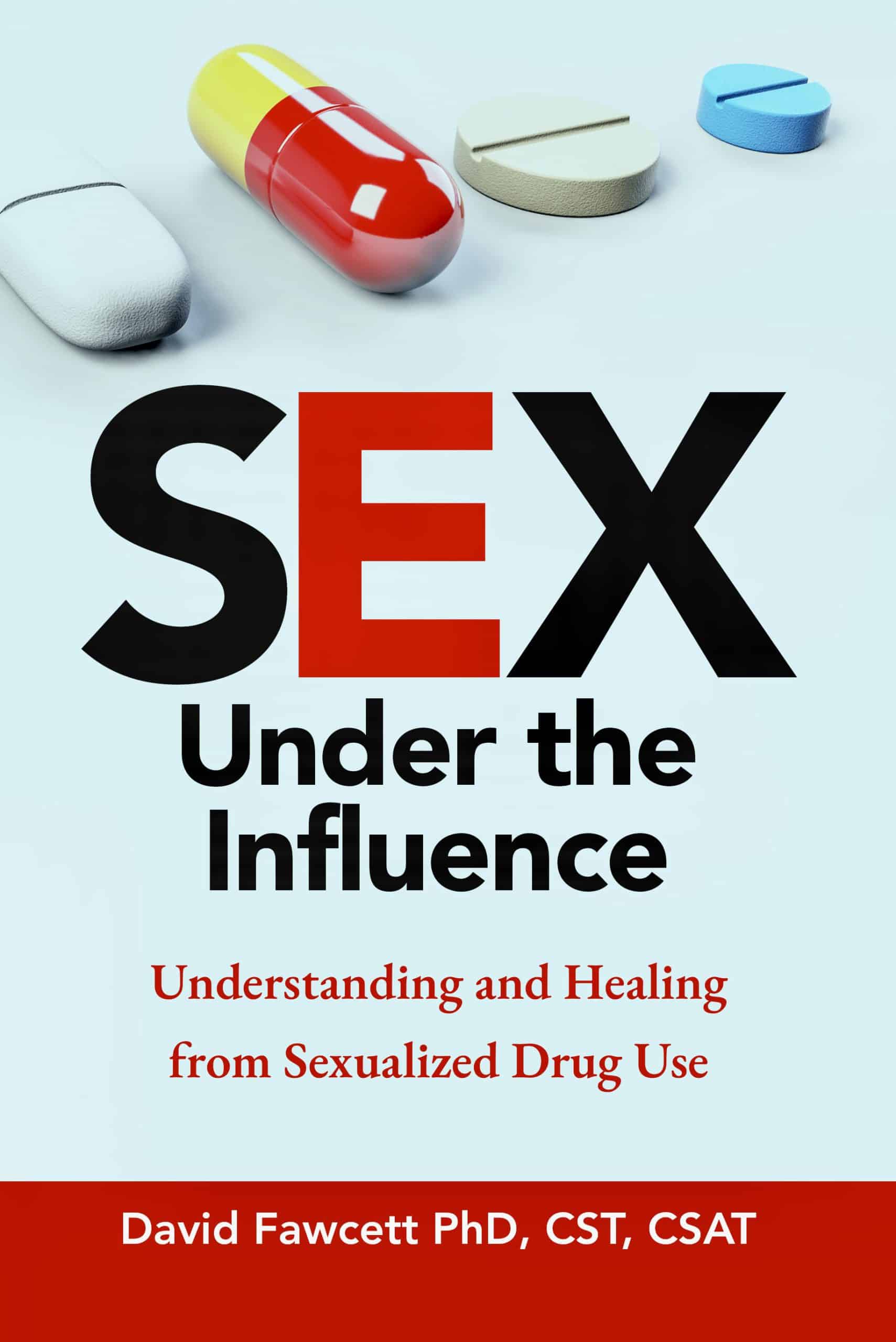
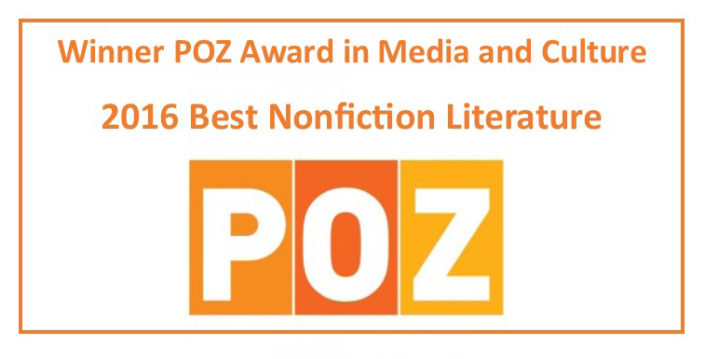
“Sex Under the Influence” Gets Worldwide Launch
Fawcett’s highly anticipated new book, “Sex Under the Influence: Understanding and Healing from Sexualized Drug Use,”...

Fawcett’s documentary “Crystal City” opens Austin’s Kink Weekend
Crystal City, the award-winning documentary, was selected to open Austin Kink Weekend in May. Fawcett, Executive...
The Gifts of Gratitude
The Gifts of Gratitude Gratitude, and the many means by which it can be practiced, is a powerful resource for anyone...
Fawcett Chairs SunServe Conference on HIV/AIDS and Seniors
Conference Highlights Challenges of Aging with HIV Individuals over the age of 50 represent half of all people living...
“Lust, Men, Meth” event is standing-room only in Seattle
On February 9, Dr. David Fawcett presented a reading and discussion on reclaiming sex and intimacy after...
Helping men deal with chemsex addiction, sex, and recovery.
Take the first step towards transformation and healing today.
Both of these books are perfect for:
- Anyone wanting to understand the impact of drugs on sexual health.
- Anyone - gay/straight, old/young, any gender, any age- struggling with combined sex and drug use.
- Health and wellness enthusiasts interested in the intersection of addiction, sexuality, and recovery.
Get the support and resources you need to create a brighter future filled with recovery and hope.
Written by a certified sex therapist, this classic book continues to help thousands of gay men around the world struggling with chemsex:
- Offers a holistic approach to recovery from meth addiction
- Provides expert insights and practical strategies for healing
- Valuable relapse-prevention skills to support your recovery journey
Order your copy today and start your journey towards recovery and healthy intimacy. Remember, recovery is possible, and you don't have to do it alone.